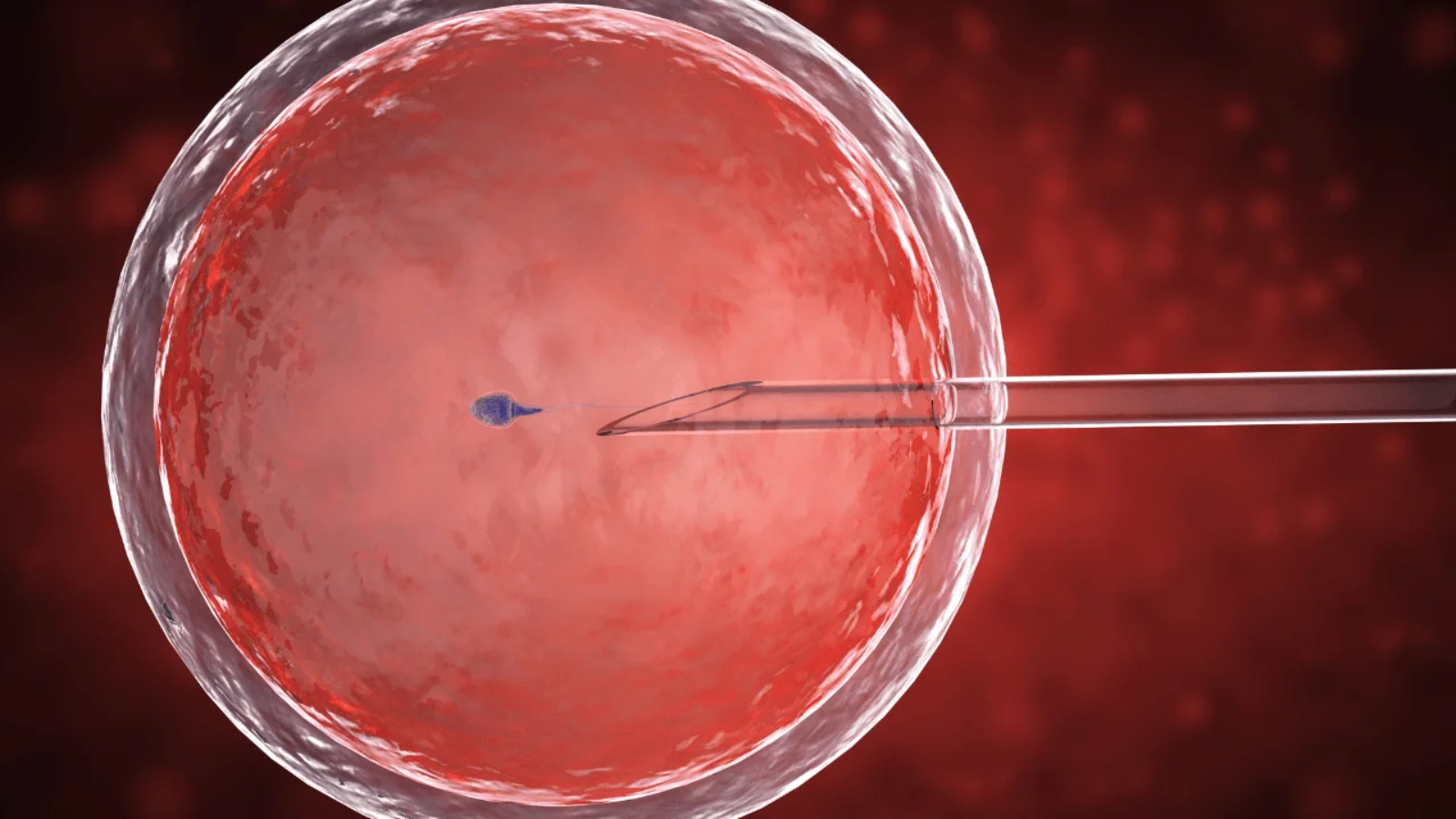
The best prenatal care begins long before egg and sperm meet up — and it starts with your preconception checkup. Before you get busy trying to make a baby, get busy making a few doctor and dentist appointments.
IN THIS ARTICLE
- How should I prepare for my preconception checkup?
- What tests and screenings will I get at my preconception appointment?
- What fertility tests might my doctor do?
- What vaccines do I need before I get pregnant?
- Other appointments to make before getting pregnant
You may not be pregnant yet, but the best way to care for your future pregnancy is to get a thorough top-to-bottom preconception checkup. A full-body tune-up now will make it easier to tackle health issues before baby’s on board and will help ensure your pregnancy is a safe and healthy one.
How should I prepare for my preconception checkup?
It doesn’t take much to prepare for your preconception checkup (other than actually making the appointment with your gynecologist), but there are a number of questions you’ll be asked during your appointment, so here’s a checklist of the information you’ll need to gather before you head to the doctor’s office:
- The type of birth control you are on. Your doctor will let you know when to stop your birth control and how long you should ideally wait, if at all, before you can start trying for that baby of yours.
- Your menstrual cycles. You’ll be asked about the date of your last period and the length of your cycles. This will help guide a discussion about your fertility and the best time each month to try to conceive.
- Your diet and lifestyle habits. Be prepared to be asked about what you eat and whether you drink or smoke. You and your doctor will discuss ways to boost your fertility through possible diet and lifestyle changes if needed.
- A list of the medications you currently take. Whether it’s over-the-counter or prescription, you and your doctor will discuss all the drugs (as well as vitamins and herbal supplements) you take. Depending on the medication (some are safe during pregnancy, others may not be), a change may be in the cards.
- Any chronic conditions or medical problems you have. Any medical problems that should be treated before conception or will need to be monitored during pregnancy are important to talk about now, so have your medical history, including your mental health history, at the ready. The good news is that with the right care and precautions, most chronic conditions are perfectly compatible with getting pregnant and having a healthy pregnancy.
- Your family history. When you’re starting a family, your family tree matters — which is why your doctor will want to check it out. Dig as deeply as you can, and write down everything you unearth, so you’ll be ready to answer the family history questions you’ll get from your practitioner. For instance, your doctor will want to know if there’s a history of breast cancer (and, depending on that answer, may recommend you get a baseline mammogram before you conceive). Your doctor will also ask about you and your partner’s family history of medical conditions (such as type 2 diabetes) and pregnancy conditions (such as preeclampsia) that might affect your pregnancy. And since multiples can run in families, be sure to share any twin trends on both your sides of the tree.
What tests and screenings will I get at my preconception appointment?
Your preconception checkup will include a lot of pre-pregnancy-specific tests and screenings, plus many of the standard screenings you’re used to from your regular annual visit. Here’s what you can expect:
- A Pap test
- A pelvic, breast and abdominal exam
- Blood pressure reading
- A weight check
- Screening for any gynecological conditions that might interfere with fertility or pregnancy, such as irregular periods, polycystic ovarian syndrome (PCOS), uterine fibroids, cysts, benign tumors, endometriosis or pelvic inflammatory disease (PID)
- A urine test to screen for urinary tract infection and kidney disease
- A blood test to check hemoglobin count (to test for anemia), vitamin D levels (to make sure you’re not deficient), Rh factor (to see if you are positive or negative), rubella titer, (to check for immunity to rubella), varicella titer (to check for immunity to chicken pox), tuberculosis (if you’re at high risk for Tb), hepatitis B titers (if you’re in a high-risk category, such as being a health care worker), cytomegalovirus titers (to determine if you’re immune to CMV), toxoplasmosis titers (if you have a cat, regularly eat raw or rare meat, or garden without gloves), thyroid function and sexually transmitted diseases
- A mental health screening for depression, anxiety disorder or any other mental health issue, including eating disorders, can interfere with conception and increase your risk of mood disorders during pregnancy and postpartum
What fertility tests might my doctor do?
If you’re under 35 and have no known fertility issues, there aren’t any additional tests in store for you at the first preconception checkup. But some doctors will be more proactive with hopeful moms-to-be over 35, testing their blood for certain fertility markers that could give a heads up on any potential difficulties in the fertility department.
These tests might include a blood test to check progesterone levels (testing around day 21 of your cycle can confirm that you’re ovulating), FSH and estradiol (testing for these two hormones on day 3 of your cycle can help indicate how many eggs you have in reserve in your ovaries) and AMH (testing for the anti-mullerian hormone also measures ovarian reserve). If your doctor suspects you might have PCOS, testing for other hormones such as testosterone and DHEA-S may be ordered.
What vaccines do I need to get before I get pregnant?
Even if you received a full set of vaccines as a child, it doesn’t mean you’re off the immunization hook now. Some vaccines require boosters to keep immunities going strong, and you want to make sure your immunity is top-notch before you get a baby on board.
The blood tests you’re getting at your preconception checkup will clue your doctor in to whether or not you have all the antibodies needed to keep you and your baby-to-be healthy during pregnancy. But it’s not just about pregnancy. Since infants aren’t fully immunized against some diseases until at least 6 months, your good health and antibodies will be vital in protecting your newborn baby’s health.
Keep in mind that once you conceive, some vaccines will be off the table, so if your antibody levels are low or you have some immunization holes that need filling in, now — before your TTC campaign begins — is the time to roll up your sleeve. Here are some vaccines that might be on your preconception agenda:
- Measles, mumps, rubella (MMR). If you’ve never been immunized against this trio of serious childhood diseases, or if testing shows your immunity wore off, you’ll need the MMR vaccine. Wait one month from the time you get the vaccine until you start trying to conceive.
- Chicken pox (varicella). If you’ve never had chicken pox or weren’t vaccinated against it, it’s recommended that you get the varicella vaccine pre-pregnancy, and that you wait at least one month before you start trying to conceive.
- Hepatitis B. If you’re at high risk for hepatitis B, it’s recommended that you get vaccinated against hepB. The hep B shots come in a series of three, and if you don’t finish up the series before you conceive, it’s safe to continue it during pregnancy.
- HPV (human papillomavirus). Are you younger than 26? If yes, you should be vaccinated against HPV with the full series of three shots before trying to conceive. If you become pregnant before completing the full series, you’ll have to resume the shots postpartum.
- COVID-19. If you haven’t gotten it yet (or you’re missing out on a booster), there’s no time like the present to gain protection. The COVID vaccine is safe and recommended for everyone 6 months and up, including women who are trying to conceive, pregnant or breastfeeding.
During pregnancy you’ll need to roll up your sleeves for two more shots: the flu shot and the Tetanus-diphtheria pertussis (Tdap) vaccine (which should be given ideally around 27 weeks to 36 weeks of pregnancy).
Other appointments to make before getting pregnant
Smile — you’re about to make a baby! And while you’re smiling, make an appointment with your dentist.
Though you probably wouldn’t normally associate your pearly whites with baby making, you’ll definitely want to schedule a dental checkup and teeth cleaning before you start trying. That’s because gum disease is associated with pregnancy complications such as preterm labor, preeclampsia and gestational diabetes.
Gum disease also tends to get worse during pregnancy, so getting your mouth in shape now is a smart idea — especially since treating gum disease before pregnancy can help reduce the risk of those complications.
If you need any work done — x-rays, fillings, crowns or gum surgery, for instance — schedule it soon so you won’t have to deal with it during pregnancy. Make sure you give yourself enough time to get it all finished up before you begin trying to get pregnant.Remember, even if you’ve never had a sick day, seeing your doctor(s) and dentist for thorough preconception checkups before you start trying to get pregnant will help ensure that all baby-making systems are go and that you’re setting yourself up for a healthy pregnancy and a healthy baby.
Read more about