
A vasectomy is a procedure that makes a man sterile by blocking his sperm. It’s a safe surgery, with minimal downtime and cost, and it’s the most effective form of birth control around with a 99.9 percent effectiveness rate. However, while reversals are occasionally successful, this is considered a permanent procedure. Anyone thinking about getting the surgery should make sure they don’t want to have any biological children in the future.
IN THIS ARTICLE
- What is a vasectomy?
- How is a vasectomy procedure done?
- Vasectomy effectiveness
- Vasectomy side effects
- Pregnancy after a vasectomy: Is it possible?
- What are the pros and cons of a vasectomy?
- What to expect during vasectomy recovery
- Are vasectomies reversible?
What is a vasectomy?
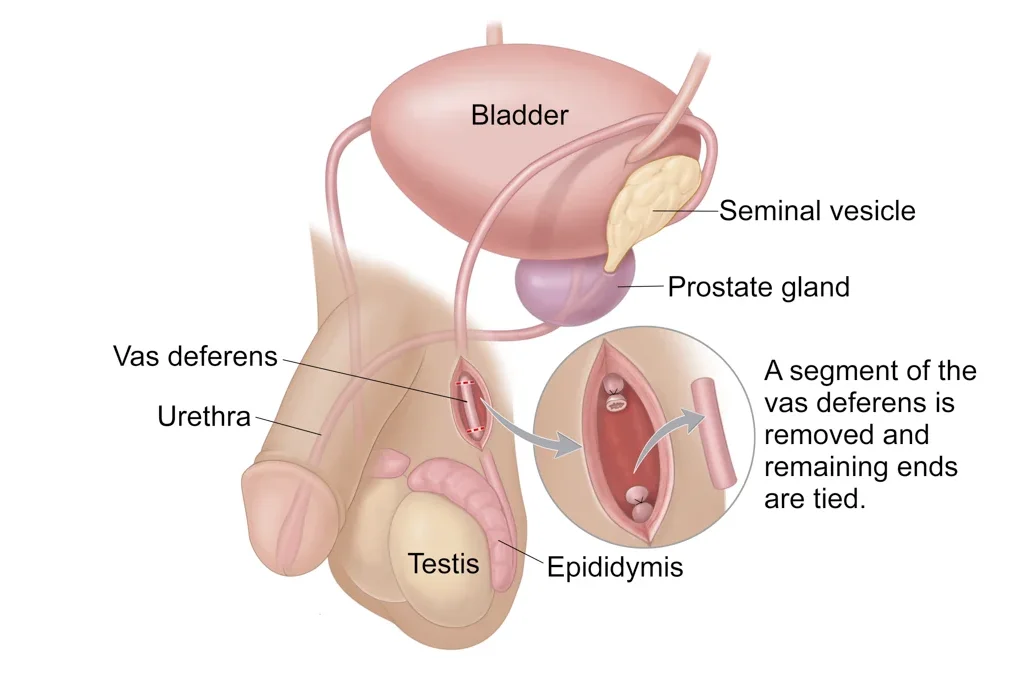
A vasectomy is a safe and highly effective procedure designed to make a man sterile. It’s done by blocking sperm from leaving the body. A doctor cuts the two tubes – called the vas deferens – that carry sperm from the testes to the pouch in the pelvis that holds the semen prior to ejaculation. Once they’re cut, sperm can’t get into the semen or out of the body. The testes still make sperm, but the sperm die and are absorbed by the body, instead of being carried into the semen.
Men who get vasectomies can still have sex and ejaculate normally, but their semen won’t contain any sperm, so it can’t fertilize an egg and cause a pregnancy.
Because the procedure is considered permanent, men will want to think carefully and consult with their provider before scheduling the procedure.
How is a vasectomy procedure done?
There are two ways the procedure can be performed. Both require only local anesthetic (numbing medicine), take only about 15 minutes, and are usually performed right in a provider’s office. (For men who aren’t comfortable having the procedure done while awake, many providers offer the procedure under a light sedation.) Here’s what to know about both:
- No-scalpel vasectomy (NSV). Most doctors today use this technique. In this procedure, the doctor gives the patient a local anesthetic and then uses their fingers to maneuver the vas deferens tubes close to the surface of the skin. Once they’re in position, they use a special instrument to make a tiny hole in the skin. When they see the tubes through that hole, they cut them and then seal them (by cauterizing or using clips). Stiches are not necessary, as the small hole will heal on its own.
- Conventional method. Some doctors prefer this approach because they feel it better enables them to see the structures they’re working with during the procedure. The doctor gives a local anesthetic and then makes a small incision on each side of the scrotum. Then, they lift the vas deferens tubes to the surface and snip them in two. Then they seal the ends (by cauterizing or using clips) and stitch up the scrotum. The stitches dissolve on their own and don’t need to be removed.
After either procedure, patients should have someone available to take them home and providers will likely recommend resting for the remainder of the day.
Vasectomy effectiveness
Vasectomy is nearly 100 percent effective. In rare cases – 1 out of 1,000 – the tubes grow back together, and the man becomes fertile again. This is one reason it’s important for men to follow up with their healthcare providers after their vasectomy to confirm the procedure was successful.
However, it’s important to note that a vasectomy is not effective immediately after the procedure. For the first 20 or so ejaculations following the vasectomy, sperm may be lingering in the tubes, so sperm count decreases gradually over time. Most providers will need to check the semen sample at least once after about three months to make sure it’s sperm-free. Until then, couples need to use another form of birth control when having sex.
Vasectomy side effects
A vasectomy is very safe, and shouldn’t cause any long-lasting side effects. There will be slight pain and swelling for the first week, but that will pass quickly, especially if taking it wasy. Pain medication such as acetaminophen may be needed. Few men have pain that doesn’t go away, but if that’s the case, a provider can check the area to make sure there are no complications.
While rare, men can xperience inflammation, bruising, or infection.
A few patients develop minor complications, such as:
- Swelling or bruising. Bleeding under the skin might cause swelling or bruising, a problem that usually clears up on its own within two to three days. If the bruise lingers, propping up the feet, applying an ice pack, and getting rest can help.
- Infection. In rare cases, the incisions or puncture wounds on the scrotum get infected. And sometimes the tubes themselves may become infected. It’s important to a provider if there’s blood or pus oozing from the site, a fever over 100 degrees Fahrenheit, or extreme pain.
- Scar tissue. Some men develop scar tissue within the scrotum that may have to be removed if it becomes painful.
- Sperm granuloma. This is a growth that develops over time in 15 to 40 percent of men who have vasectomies. It happens because the body’s immune system reacts to leaking sperm at the end of the cut vas. It’s not dangerous and is usually treated with ibuprofen if uncomfortable. Rarely (if it becomes very uncomfortable), it may need to be surgically removed.
- Discoloration of the scrotum. This generally occurs as a result of a bruise or swelling, and will quickly dissipate over time with ice and rest.
More rarely, men who have vasectomies might:
- Develop post-vasectomy pain syndrome. This dull ache in the testes is caused by the buildup of fluid or by damage to the nerves surrounding the vas. It’s usually treated with ibuprofen and warm baths. In severe cases, other oral medication, steroid injections, nerve blocks, or surgery might be needed. This syndrome affects between 1 and 2 percent of men who have a vasectomy, and it’s always treatable.
- Develop a hydrocele. This is a fluid-filled sac that causes swelling in the scrotum. Treatment usually isn’t necessary, but if the hydrocele is large and uncomfortable, it can be surgically removed. Most hydroceles have nothing to do with vasectomies.
- Develop epididymitis. The epididymis is a duct located behind the testicles, and it allows sperm to flow to the vas deferens. When a man has a vasectomy, sperm can still flow from the epididymis to the vas deferens, but becomes backed up because the vas deferens has been cut. In some men, this can cause inflammation of the gland (about 1 to 3 percent).
- Develop a vasovenous fistula. A vasovenous fistula is a very rare complication of vasectomy, which occurs when multiple blood vessels adhere to the vas deferens, and then become injured. This can result in the pooling of blood that leads to the development of a fistula – aka, an abnormal connection between the vas deferens and nearby blood vessels. Symptoms of a vasovenous fistula may include blood in urine or ejaculate. Men will need to call their healthcare providers immediately if theyexperience this.
There’s no evidence that the procedure increases the chances of prostate cancer, testicular cancer, or developing heart disease, as some people once thought. In fact, there are no known long-term side effects relating to overall health and sexual activity besides those mentioned above.
It’s very important to note that a vasectomy does not affect a man’s sex life. Men sometimes jokingly use a high-pitched voice when discussing vasectomy. The procedure, however, has no effect on a man’s voice, testosterone production, facial hair, sex drive, or sexual functioning. (It doesn’t affect the ability to get an erection, ejaculate, or orgasm.)
The vas deferens carries nothing but sperm, so the operation simply keeps these cells out of the semen. (They’re then reabsorbed into the body.) The sperm actually make up only a very small part of the semen, with most of the fluid coming from the prostate gland. Therefore, vasectomy won’t make a major change in the amount of fluid that comes out with ejaculation, and men won’t know the difference.
Pregnancy after a vasectomy: Is it possible?
While it’s certainly possible, it’s very rare to get pregnant post-vasectomy, as it’s considered one of the most effective forms of permanent birth control – in fact, surveys suggest that there is only about 1 pregnancy per 1,000 vasectomies, making it a 99.9 percent effective procedure.
The biggest chances of getting pregnant after a vasectomy occur in the three months right after, when there still may be some sperm left in the semen. If the surgery fails, there is also a chance of pregnancy, but this is extremely rare.
What are the pros and cons of a vasectomy?
Pros
A vasectomy is a good choice for men and their parterns who are sure they don’t want to conceive any more children/ The main benefits are convenience and freedom: Men don’t have to put on a condom every time you want to have sex, and their partners won’t have to take a pill every day or insert or apply anything before having sex. This may help increase intimacy in the relationship.
Another plus: The surgery will save money in the long run. Once you’ve paid for the procedure, you’ll have no additional contraceptive expenses.
Vasectomies are safer, easier to recover from, and cheaper than the female sterilization equivalent.
Cons
The procedure is not for men who think they might change their mind. The cost of reversing the procedure is high, and there’s no guarantee of success. (If the reversal procedure is unsuccessful, sperm can sometimes be collected from the testicle to use for in vitro fertilization (IVF), but this is also a costly procedure.)
Before you go under the knife, men will want to ask themselves some tough questions: How would they feel if they lost their partner to death or through divorce or separation and later decided to have a child with another person – or if anything happened to their living children? It’s important to try and imagine all possible scenarios that might make one change their mind.
Also, sterilization doesn’t protect men from sexually transmitted infections such as HIV, herpes, HPV (genital warts), syphilis, gonorrhea and chlamydia.
What to expect during vasectomy recovery
Recovery from a vasectomy is pretty quick. In a week’s time, men who have a vasectomy should be fully recovered, and most will likely feel better much before then. Most men are able to return to work in about two or three days, exercise within seven days, and have sex again in a week.
In the meantime, these techniques can ease discomfort:
- Ice. Using an ice pack (or a bag of frozen peas) on the scrotum (on top of the underwear or wrapped in a towel) can reduce swelling. (It’s a good idea to bring an ice pack with to the doctor’s office, along with a jock strap to help support the scrotum after the procedure).
- Loose bandages and underwear. Doing this for at least 48 hours after surgery can help make things easier on the scrotum.
- Pain relief. If the soreness is uncomfortable, men can take acetaminophen, but not ibuprofen or aspirin, because these may increase the risk of bruising or bleeding. It’s not common, but if there’s intense pain during this time, a healthcare provider may suggest pain medication to help control it.
- Rest. Planing to lie around for a few days is best. Men will need to wait a day or two to bathe or swim, and it’s wise to wait a week or so before having sex, lifting heavy objects, riding a bike, jogging, golfing, or engaging in other strenuous activities. Men who have the operation on Friday can probably return to work Monday, unless their job involves physical labor.
Are vasectomies reversible?
A vasectomy can be reversed, but it’s an expensive and much more involved procedure (which can take over three hours, often under general anesthesia.) It’s rarely covered by insurance. TOnly those who are certain their done having children should have this procedure.
However, there are two ways in which a surgeon can attempt to reverse a vasectomy, and it involves reconnecting the vas deferens, which allows sperm to enter the semen.
- Vasovasostomy. A surgeon reattaches the two ends of the vas deferens using a high-powered microscope to view the tiny tubes.
- Vasoepididymostomy. A surgeon attaches the top end of the vas deferens directly to the epididymis, which is a tube in the back of the testicle.
The surgeon will usually decide which approach is best, and it could be a combination of the two.
The reversal procedure often doesn’t work, and the more time that has elapsed since the vasectomy, the smaller the chance that a reversal procedure will make a man fertile again. This is partly because the vas deferens may deteriorate over time and partly because some men develop antibodies to their own sperm after a vasectomy, making the sperm less effective.
A vasectomy reversal’s success can also depend on other factors, such as age, and the surgeon’s experience. As a back-up plan, men can talk to their healthcare providers about putting some of their sperm in a sperm bank.
Read more about


Add a Comment