Fertility Treatments. Researching fertility treatments? Start here. This overview of the most common fertility treatments available, including IUI and IVF, will help you understand your options and decide on next steps.
IN THIS ARTICLE
- Intrauterine insemination (IUI)
- In vitro fertilization (IVF)
- Donor eggs
- Gestational carrier (surrogacy)
- Egg freezing
- Fertility drugs
If you and your partner are among the 12 percent of couples who deal with infertility, you know that coping with problems conceiving can be hard. And though fertility treatments can go a long way towards helping you get pregnant, there’s a good chance that navigating all the options might just add to your stress level.
But having a quick overview of the choices can help. Use this guide to learn the basics of the most common fertility treatments. Once you get a feel for what might be right for you, you can discuss them with your doctor and do a deeper research dive to get more specifics.
Intrauterine insemination (IUI) Fertility Treatments
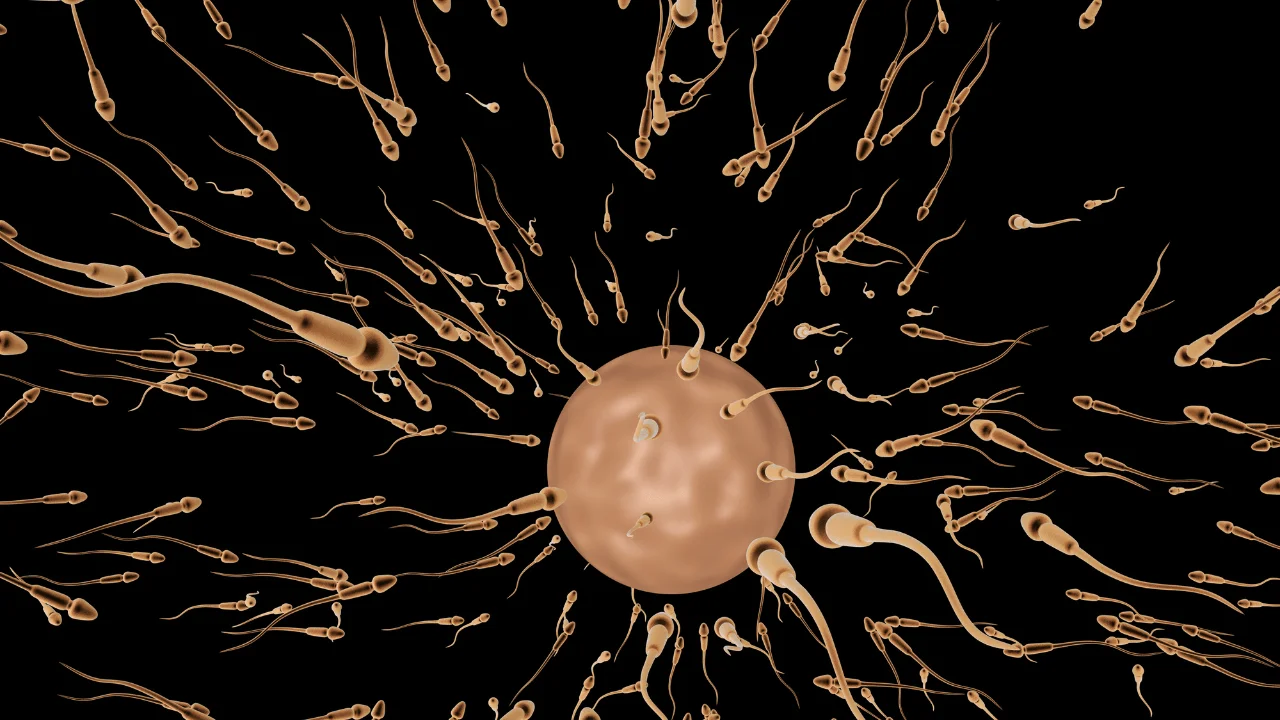
With intrauterine insemination (IUI), a thin catheter is used to place sperm directly in the uterus close to the fallopian tubes, upping the chances that sperm will meet egg. It involves placing sperm from your partner or a donor inside your reproductive tract during ovulation to help you get pregnant.
If you’re ovulating normally, AI can be done without any additional fertility drugs. If you’re having issues with ovulation, doing IUI with fertility drugs can boost your chances of getting pregnant.
Can be good for: These procedures may be right for couples dealing with lower sperm counts or poor sperm motility, same-sex couples or single women who want to become moms on their own. IUI is also a good first option for those with unknown fertility issues.
Success rates: Up to 40 percent of women under the age of 40 who undergo AI will get pregnant within six tries. For IUI, the success rate ranges from 5 to 15 percent per try.
Side effects or risks: There are no real risks to IUI, other than a rare chance of developing an infection, but the procedure won’t work for everyone. IUI is less likely to be effective for women over 40, as well as those with fallopian tube blockages, a history of pelvic infections or significant endometriosis.
It also likely won’t work for male infertility problems including very low sperm count or significant problems with sperm motility or morphology (the percentage of sperm that appear to be of normal shape and size).
In vitro fertilization (IVF)
During IVF, your eggs are fertilized by sperm in a laboratory or fertility clinic. Then one or more of the embryos (fertilized eggs) are transferred into your uterus with the hope that it’ll implant and result in a pregnancy.
Can be good for: Your doctor might recommend IVF if IUI hasn’t been successful for you. IVF can also be a good choice for those dealing with severe fallopian tube blockages, ovulation problems, diminished ovarian reserve, polycystic ovary syndrome (PCOS), endometriosis or severe sperm factor. Same-sex couples, couples using donor eggs or any couple that might need to use preimplantation genetic diagnosis or screening (PGD/PGS) to screen embryos for genetic disorders would use IVF, too.
Success rates: Success rates for IVF vary depending on a woman’s age, and can range from 12 to 70 percent.
Side effects or risks: You’ll need to take hormone shots before your eggs can be harvested for fertilization, which can cause unpleasant side effects. The procedure itself is invasive, and implanting more than one fertilized egg also makes you more likely to have twins or multiples, which ups the odds for possible complications. Plus, it can be expensive if not covered by insurance.
Donor eggs
The process involves fertilizing a donor egg with sperm and implanting it into your uterus, similar to IVF. The donor can be someone you know or someone you are matched with anonymously through an agency.
Using a donor egg means you won’t be related to your baby biologically — but you’re still listed as the birth mother on record.
To avoid any legal pitfalls, hire a lawyer early in the process to make sure you have a formal contract between you and your donor and/or the donor agency waiving all parental rights and outlining that any children born from the donated eggs are legally yours.
Can be good for: If traditional IVF cycles haven’t worked, donor eggs can be a next step. The procedure also might be right for women with a low egg count or poor egg quality, which is more likely after age 40. Donor eggs are also an option if you have a genetic disorder or serious condition that you want to avoid passing on to your child.
Success rates: Around 50 to 70 percent when fresh donor eggs are used and around 40 to 60 percent when frozen donor eggs are used.
Side effects or risks: Using donor eggs can be a lengthy and expensive process, and for some women, coming to terms with the fact that they won’t have a genetic link to their baby can be emotional. And as with traditional IVF, there’s a risk of multiples and related complications.
Gestational carrier (surrogacy)
A gestational carrier (GC), also called a gestational surrogate, carries a child for another woman or same-sex couple. In virtually all cases, the parents undergo IVF and the embryo is implanted in the surrogate’s uterus. Both parents have a genetic tie to the baby, but the surrogate doesn’t.
Can be good for: Using a GC can be a good option for couples who want a biological child but can’t carry a pregnancy. Same-sex couples or women who can’t sustain a pregnancy, don’t have a uterus or have a medical condition that would make pregnancy dangerous or impossible might also consider GC
Success rates: Rates are similar to rates of women using their own uterus and depend on the age of the woman whose eggs were used to create embryos.
Side effects or risks: Being a GC can be an intensely emotional process that can take 18 months or more. There are also major legal aspects to deal with: It’s in the best interest of parents and surrogates to have a contract spelling out details like parental rights and custody, as well as medical treatment during pregnancy and labor and delivery. And it’s important to note that surrogacy is currently illegal in some states, and some states do not recognize surrogacy contract agreements. Be sure to check your state laws.
Egg freezing
Egg freezing involves retrieving a woman’s eggs in a procedure similar to IVF, then freezing and storing them. When you’re ready to have a baby, the eggs are thawed, fertilized and implanted into your uterus.
Can be good for: Egg freezing might be worth considering if you know that you want children at some point but not for a while. It can also be a good option for women undergoing cancer treatment or those with a family history of early menopause, endometriosis or ovarian cysts. Women in their 20s and early 30s have the best chance of retrieving, freezing and storing healthy eggs.
Success rates: The data is limited, but the chances of one frozen egg resulting in a successful pregnancy are around 5 to nine percent per egg frozen for women under 38. The older you are when you freeze your eggs, the lower the odds of successful fertilization later.
Side effects or risks: Since the vast majority of women who’ve frozen their eggs haven’t used them yet, experts don’t know much about how long frozen eggs will last in storage. Also, as with traditional IVF, you have to take fertility drugs, which can have unpleasant side effects, and the procedure itself is invasive.
Fertility drugs
Fertility drugs are taken at the start of IVF, but you can also take them on their own for ovulation issues.
Oral meds like Clomid and letrozole are used to stimulate the ovaries and correct irregular ovulation. Both drugs work by suppressing estrogen production, which boosts the production of ovulation-stimulating hormones. If oral medications don’t work, there are hormone shots called gonadotropins that directly stimulate ovulation.
If your irregular ovulation is caused by polycystic ovary syndrome (PCOS), the drug Metformin can also be an option. While it’s normally used to treat diabetes, Metformin works to sensitize insulin levels, which can help women with PCOS achieve more regular ovulation.
Can be good for: If intrauterine insemination (IUI) hasn’t worked for you, it might be more successful with fertility drugs. You can also take fertility drugs while trying to conceive on your own without IUI or IVF. Fertility drugs can be a particularly good choice for women with ovulation issues related to PCOS. In fact, the American College of Obstetricians and Gynecologists (ACOG) recommends letrozole as a first-line treatment for PCOS-related infertility.
Success rates: Successful pregnancy rates with fertility medications depend on the drug. For hormone shots it’s 32 percent, for letrozole it’s 28 percent and for Clomid it’s 23 percent. Among women with PCOS, not all studies show that taking Metformin improves the chances for getting pregnant through IVF, but a recent analysis suggested it could increase the odds specifically for women with a body mass index greater than 26.
Side effects or risks: You might experience side effects such as bloating, nausea, headaches, mood swings or breast tenderness. Hormone shots also come with a slight risk of ovarian hyperstimulation syndrome, where the ovaries become swollen and painful. Fertility drugs increase the odds for multiples, too, since they could cause two or more eggs to be released at a time. If you and your partner need help conceiving, there are a number of options. Together, think about the ones that seem like they might be a good fit, then talk with your doctor to figure out a plan you feel comfortable with.
Read more about


Add a Comment