Artificial Insemination. Overcoming fertility challenges doesn’t always mean complicated surgeries or high-tech procedures. In some cases, a couple needs just a little extra help to make the miracle of conception happen.
IN THIS ARTICLE
- What is artificial insemination (AI)?
- What is intrauterine insemination (IUI)?
- What’s the difference between IUI and IVF?
- Who’s a candidate for artificial insemination or IUI?
- How is IUI done?
- Can you do artificial insemination at home?
Back when you first started trying to conceive, you probably knew that conception wouldn’t happen overnight. But you were pretty confident it would happen — and that it would happen in the privacy of your own bedroom.
Fast forward to now, following test after test — and perhaps even a few rounds of fertility medication — and it may be time to try something new.
Enter artificial insemination (AI) or intrauterine insemination (IUI) — one of the oldest and simplest assisted reproduction techniques, and still one of the most successful ones.
What is artificial insemination (AI)?
Artificial insemination, or AI, is a fertility treatment that places your partner’s (or a donor’s) sperm inside your reproductive tract when you’re ovulating to help promote conception.
AI aims to give sperm a better chance of reaching Destination Egg by bypassing the initial hurdles they would encounter in the vagina and cervix — sort of a running (or swimming) head start.
What is intrauterine insemination (IUI)?
Intrauterine insemination, or IUI, is a type of AI in which sperm are placed directly into the uterus close to the fallopian tubes, where fertilization takes place.
The goal: to get those sperm as close as possible to their target — your waiting egg — so they can be at the right place at the right time.
Skipping the trip through the vagina and the cervix cuts down on the swimming sperm have to do, making it more likely that they’ll reach the egg on time.
What’s the difference between IUI and IVF?
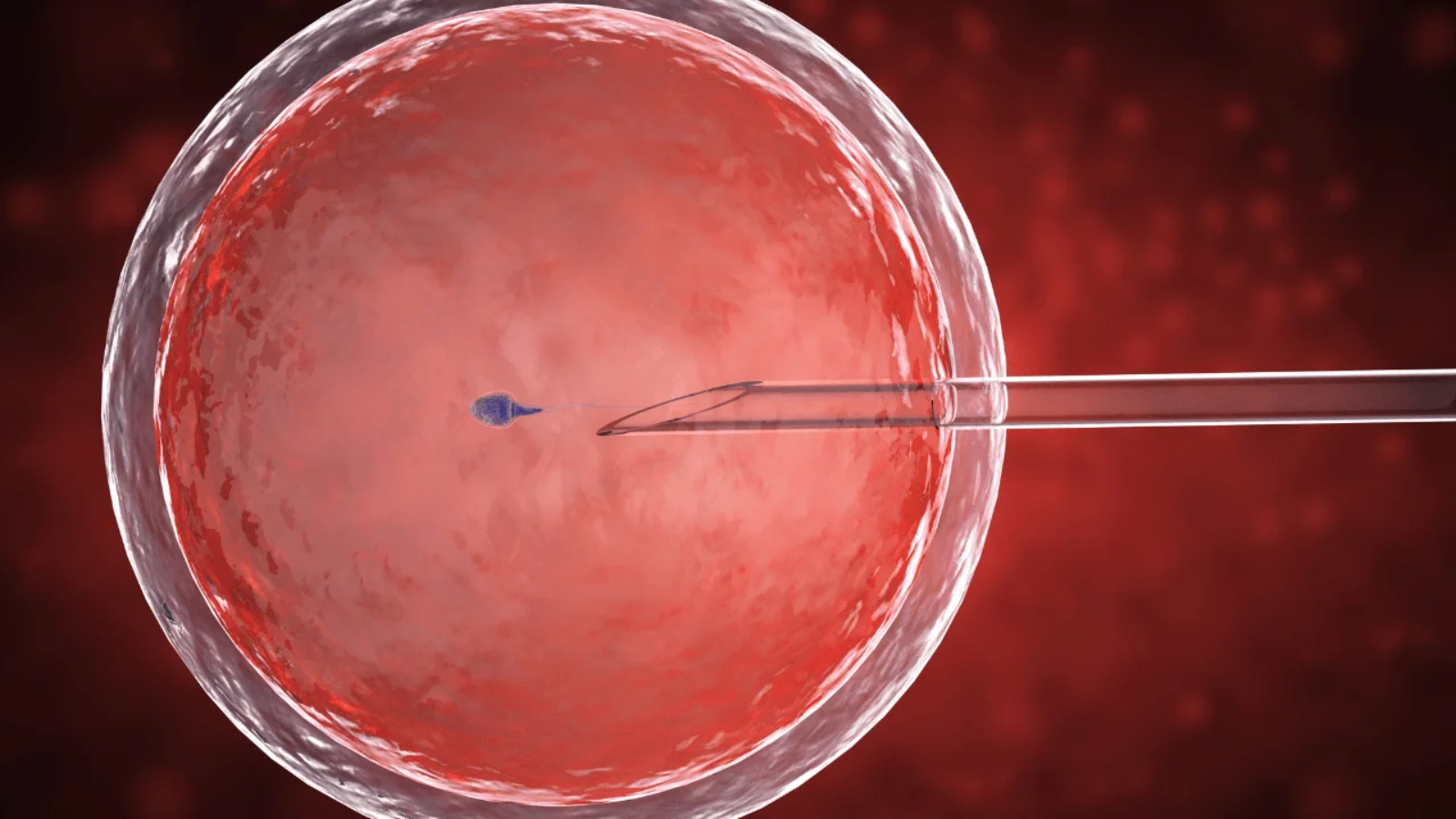
In IUI, the sperm are inserted directly into your body (specifically, the uterus) in the hopes of fertilizing an egg. During in vitro fertilization (IVF), an egg is fertilized with sperm in a laboratory, then transferred back into the uterus.
Whereas an IUI procedure takes only a few minutes, an IVF cycle can take a month or more to complete.
With IVF, you’ll likely need to get hormone shots to stimulate your ovaries and will get a human chorionic gonadotropin (hCG) injection or another drug to help your eggs mature.
The eggs will then be retrieved using an ultrasound-guided needle, and fertilized with your partner or donor’s sperm. After three to five days, the embryos can be transferred into the uterus.
Women may want to try IVF if they have severe blockages in the fallopian tubes, poor egg quality or endometriosis.
Who’s a candidate for artificial insemination or IUI?
Couples experiencing otherwise unexplained fertility issues, where it’s clear nature could use a nudge, are good candidates for IUI.
Couples with mild male factor fertility problems are also good candidates. This assisted reproductive technique can also help when the cervical environment or cervical mucus is hostile to sperm, making it hard for them to swim.
Same-sex couples may also turn to artificial insemination for help starting their family (either themselves or with a surrogate), as can single women who want to become moms on their own with a sperm donor.
IUI isn’t recommended for women who have significant fallopian tube blockages or conditions, a history of pelvic infections or severe endometriosis.
Does your guy have a very low sperm count, or significant problems with sperm motility or morphology (the percentage of sperm that appear to be of normal shape and size)? Fertility specialists will usually not recommend IUI in those situations, since it’s less likely to be successful.
How is IUI done?
IUI is done in the doctor’s office, during a visit timed to correspond to when you’re ovulating.
Ovulation may be induced with Clomid or another ovulation induction medication, though for women who don’t need the extra help, the procedure can be timed to correspond with your natural window, in what’s called a natural-cycle IUI.
Here’s what to expect during the procedure:
- First you’ll lie on the exam table with your feet in stirrups — the same position as for a pelvic exam.
- The doctor will take a concentrated sperm sample from your partner or donor and inject it into your uterus through a thin, flexible catheter placed into the vagina and through the cervix. Because the procedure is done when you’re ovulating, your cervix will already be slightly open, making the insertion of the catheter and injection of the healthy sperm easier.
- Once the insemination is complete, you’ll be asked to lie on your back for a brief period, and then you’ll be able to return to regular activity.
The whole IUI procedure takes only a couple of minutes, and there isn’t much discomfort — or, about as much as you’d have during a Pap test. There’s also no need to worry if you experience light spotting for a day or two after your IUI — that’s normal for some women.
A few notes about the sperm used in IUI: This sperm isn’t “fresh” — it’s been washed in preparation for the procedure, optimizing the sperm to maximize the odds of fertilization.
Because sperm is inserted directly into the uterus during IUI, it bypasses the cervical mucus. The washing process accomplishes what the cervical mucus would normally do, separating sperm from the semen, separating nonmotile sperm from motile sperm and purifying the sperm by removing potentially toxic substances and fluid.
For at least 48 hours before the procedure, sex and ejaculation will be off the table for your partner or donor. He’ll provide his sperm sample, either in the clinic’s collection room or at home, on the same day as your IUI, making sure that the sperm sample is handed over within an hour or so of the IUI.
If you’re using donor sperm or your partner’s previously frozen sperm, it will be thawed immediately before the IUI procedure. The insemination then takes place as soon as the sperm washing is complete.
Right now, IUI is the gold standard of artificial insemination — and the go-to AI procedure.
Can you do artificial insemination at home?
At-home insemination is attractive to some trying-to-conceive couples who’d like to skip the fertility doctor (and the resulting bills) if possible. For heterosexual couples, at-home AI offers no fertility edge over regular sex. But single women or same-sex women couples may want to try at-home AI before turning the insemination process over to a doctor.
There are a few at-home options: There’s the “turkey baster method” — in which you inject freshly ejaculated semen into the vagina (close to the cervix) using a needleless syringe. Or you can fill a cervical cap, diaphragm, or a period collection cup with semen and insert it over your cervix, leaving it in place for two to three hours.
There are also at-home AI kits. As with IUI, timing is everything with at-home AI: You’ll need to inject the sperm as close to ovulation time as possible. And just as with any artificial insemination technique, an at-home AI won’t be effective if you have ovulation problems or if your partner has a very low sperm count or poor-quality sperm.
There are some potential risks with at-home AI: tissue damage, uterine perforation and even infection if the insertion is too deep or done improperly.
Be aware, too, of potential legal risk if you’re using donor sperm for an at-home AI, since the legal protections afforded by medically supervised donor sperm used for IUI in a fertility clinic — things like the automatic termination of the donor’s parental rights — don’t always cover women who artificially inseminate at home. The laws vary from state to state, so do check your state’s statutes before you do it yourself.
Read more about